STORY AT-A-GLANCE
- According to British deputy chief medical officer Dr. Jenny Harries, the evidence for face masks is “not very strong in either direction.” Sweden’s coronavirus pandemic response leader, Dr. Anders Tegnell, dismisses the scientific evidence for mask-wearing, calling it “astonishingly weak”
- White House coronavirus task force coordinator Dr. Deborah Birx is urging Americans to wear their mask whenever they’re around others, including other household members, while admitting that “when people start to realize that 99% of us are going to be fine,” compliance becomes “more and more difficult”
- A 2015 study found health care workers wearing cloth masks had a 72% higher rate of laboratory-confirmed respiratory virus infections, when compared to those wearing medical masks or controls (who used standard practices that included occasional medical mask wearing)
- A working paper by the National Bureau of Economic Research (NBER) suggests draconian lockdown measures implemented in many countries, including the U.S., have achieved little in terms of stemming the death toll; regardless of policy, deaths per day stop increasing within 20 to 30 days of passing a threshold of 25 deaths
- According to the NBER, lockdowns, closures, travel restrictions, stay-home orders, event bans, quarantines, curfews and mask mandates do not seem to affect virus transmission rates overall, and governments have likely acted in error
According to an August 28, 2020, article1,2 in The Telegraph, British Prime Minister Boris Johnson now “insists he does not want to see face coverings in schools.” During a question and answer session posted on Facebook, Johnson said:3,4
“There’s no need for it. Indeed, there’s a need not to have it because obviously it’s very, very difficult to teach or to learn with a face mask on.”
British deputy chief medical officer Dr. Jenny Harries stated the evidence for face masks is “not very strong in either direction,” but that advice may change in the future should scientific evidence emerge. For now, head teachers will be allowed to make their own decisions about mask adherence in school hallways and communal areas.
“Dr. Harries said that the wearing of masks in hallways and communal areas ‘can be very reassuring in those enclosed environments’ despite the lack of definitive science,” The Telegraph reports, adding:5,6
“She also urged people to be ‘very kind’ to those with disabilities who were ‘struggling’ with coronavirus measures such as the wearing of face coverings. ‘Many of the actions that we have quite rightly taken to control the pandemic can be quite difficult for people with all sorts of sensory disabilities,’ she admitted.”
Sweden’s Pandemic Response to Masking
Sweden is one of the few countries where draconian pandemic responses have not been widely implemented. Throughout the pandemic, most of the country’s businesses have remained open, and people have to a large degree been allowed to go about their lives as usual, albeit with the general recommendation to social distance whenever possible.
According to an August 10, 2020, article7,8 in The Times, the epidemiologist in charge of Sweden’s coronavirus pandemic response, Dr. Anders Tegnell, “has dismissed the scientific evidence for mask-wearing as ‘astonishingly weak’ and suggested that making face coverings mandatory could backfire.”
Tegnell insists the only viable solution in the long run is to trust people and give them the responsibility to make sensible decisions for themselves.
“It is a Swedish tradition that we give a lot of responsibility to individuals and influence them. So, we never saw any reason to take more drastic measures … I’m surprised that we don’t have more or better studies showing what effect masks actually have.
Countries such as Spain and Belgium have made their populations wear masks but their infection numbers have still risen. The belief that masks can solve our problem is in any case very dangerous,” Tegnell said in a recent interview with a German newspaper.9,10
Interestingly, despite the country’s lack of lockdowns and mandatory mask requirements, infections have now “dwindled away to a negligible level” on their own.
According to The Times, as of August 10, 2020, Sweden’s total death toll for COVID-19 stood at 5,763. At the peak of the pandemic in mid-April, just under 100 daily COVID-19 related deaths were recorded. By early August, the average death toll was down to one or two per day. Positive test results are also trending downward.
Birx Ridiculously Urges Mask Wearing at Home
Meanwhile, in the U.S., the fact that the curve has been flattened and the total COVID-19 death rate has been dramatically reduced11 doesn’t seem to make a difference. At the end of August, White House coronavirus task force coordinator Dr. Deborah Birx urged Americans to stay vigilant, and to wear their mask whenever they’re around others, including other household members. According to CNN:12
“Birx urged Americans to take personal responsibility, especially if they want to help keep economies open. ‘Right now, we gain freedom through wearing our masks and socially distancing,’ she said.”
Ironically, in mid-August, during a visit to Little Rock, Arkansas, Birx gave the following statements, reported by Eldorado News-Times:13
“‘I’ve been so struck by the number of Americans across the country that have just had it,’ she said. ‘Mortality decreases’ have also complicated matters … ‘When people start to realize that 99 percent of us are going to be fine, it becomes more and more difficult’ to get people to comply, she said.”
What Is the Real Risk of COVID-19 at This Point?
Indeed, it now appears the mortality rate of COVID-19 may be right around or lower than that of influenza. During an August 16, 2020, lecture at The Doctors for Disaster Preparedness14 convention, Dr. Lee Merritt15 pointed out that, based on deaths per capita — which is the only way to get a true sense of the lethality of this disease — the death rate for COVID-19 is around 0.009%.
That number is based on a global total death toll of 709,000, and a global population of 7.8 billion. This also means the average person’s chance of surviving an encounter with SARS-CoV-2 is 99.991%. The U.S. area with the highest death rate, New York, has a death per capita rate of 0.17%. Merritt’s lecture with this information is featured in “How Medical Technocracy Made the Plandemic Possible.”
So, while mainstream media still claims a mortality rate below 1% is a complete hoax, Birx verified — whether on purpose or by accident — that at least 99% of the population has nothing to fear from this virus.
And remember, the total death toll is enormously falsely inflated with those that died WITH, rather than FROM, SARS-CoV-2. The reason the U.S. Centers for Disease Control hasn’t ended COVID-19’s epidemic status also appears to be because they include deaths from pneumonia and influenza in the statistics. Combined, pneumonia, influenza and COVID-19 deaths were still above the epidemic threshold, based on data through August 22.16
Meanwhile, deaths in which COVID-19 is listed on the death certificate as the sole cause of death are only 6% of the total COVID-19 death toll, according to CDC data released August 26.17 On that day, the total death toll listed was 161,392, 6% of which would be 9,683.
The remaining 94% had an average of 2.6 “additional conditions or causes” contributing to those deaths. That even includes 5,133 deaths from intentional or unintentional injuries (according to the data listed on August 26; exact numbers may have changed since then).
Evidence Shows Masks Do Not Protect Against Viral Infection
I’ve already written several articles detailing studies showing that masks cannot protect against viral infections. The reason is simple. SARS-CoV-2 has a diameter of 0.06 to 0.14 microns.18 Medical N95 masks — which are considered the most effective — can filter particles as small as 0.3 microns.19 Surgical masks, homemade masks, T-shirts and bandanas are even more porous.
Strangely, mask mandates continue to flourish despite health agencies own research showing it’s a futile measure that only provides a false sense of security:
- The World Health Organization’s June 5, 2020, guidance memo20 on face mask use states “there is no direct evidence (from studies on COVID- 19 and in healthy people in the community) on the effectiveness of universal masking of healthy people in the community to prevent infection with respiratory viruses, including COVID-19.”
- According to a policy review paper21 published in the CDC’s own journal, Emerging Infectious Diseases, in May 2020: “Our systematic review found no significant effect of face masks on transmission of laboratory-confirmed influenza.”
- The National Academies of Sciences in its Rapid Expert Consultation on the Effectiveness of Fabric Masks for the COVID-19 Pandemic report,22 published April 8, 2020, concluded “The evidence from … laboratory filtration studies suggest that … fabric masks may reduce the transmission of larger respiratory droplets,” but that “There is little evidence regarding the transmission of small aerosolized particulates of the size potentially exhaled by asymptomatic or presymptomatic individuals with COVID-19.”
Researchers Warn Against Cloth Masks
A study published in 2015 recently received additional commentary from the authors in light of the COVID-19 pandemic. The original study23 was titled “A Cluster Randomized Trial of Cloth Masks Compared with Medical Masks in Healthcare Workers.”
They found that health care workers wearing cloth masks had the highest rates of influenza-like illness and laboratory-confirmed respiratory virus infections, when compared to those wearing medical masks or controls (who used standard practices that included occasional medical mask wearing). Compared to controls and the medical mask group, those wearing cloth masks had a 72% higher rate of lab-confirmed viral infections. According to the authors:
“Penetration of cloth masks by particles was almost 97% and medical masks 44%. This study is the first RCT of cloth masks, and the results caution against the use of cloth masks. This is an important finding to inform occupational health and safety.
Moisture retention, reuse of cloth masks and poor filtration may result in increased risk of infection. Further research is needed to inform the widespread use of cloth masks globally. However, as a precautionary measure, cloth masks should not be recommended for HCWs [health care workers], particularly in high-risk situations …”
In a follow-up commentary dated March 30, 2020, the authors of this study address questions received during the pandemic from health care workers concerned about instructions to use cloth masks if or when medical-grade masks are unavailable. Their comment reads, in part:24
“The study found that cloth mask wearers had higher rates of infection than even the standard practice control group of health workers, and the filtration provided by cloth masks was poor compared to surgical masks …
Health workers are asking us if they should wear no mask at all if cloth masks are the only option. Our research does not condone health workers working unprotected. We recommend that health workers should not work during the COVID-19 pandemic without respiratory protection as a matter of work health and safety …
There have been a number of laboratory studies looking at the effectiveness of different types of cloth materials, single versus multiple layers and about the role that filters can play. However, none have been tested in a clinical trial for efficacy.
If health workers choose to work using cloth masks, we suggest that they have at least two and cycle them, so that each one can be washed and dried after daily use. Sanitizer spray or UV disinfection boxes can be used to clean them during breaks in a single day. These are pragmatic, rather than evidence-based suggestions, given the situation.
Finally for COVID-19, wearing a mask is not enough to protect healthcare workers — use of gloves and goggles are also required as a minimum, as SARS-CoV-2 may infect not only through the respiratory route, but also through contact with contaminated surfaces and self-contamination.”
Pandemic Policies Have Achieved Little
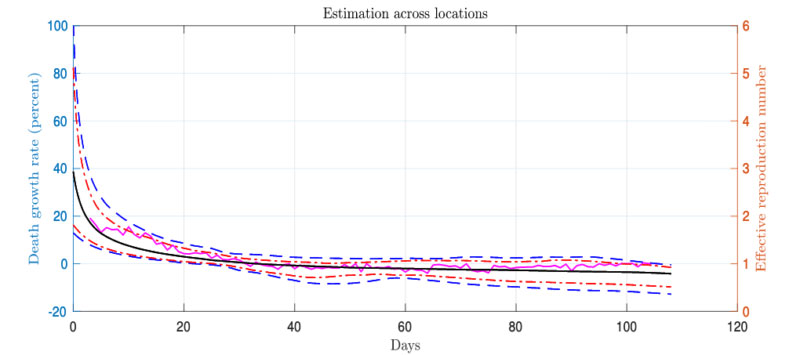
Last but not least, a working paper25 by the National Bureau of Economic Research (NBER), written by Andrew Atkeson, Karen Kopecky and Tao Zha, suggests the draconian lockdown measures implemented in many countries, including the U.S., have achieved little in terms of stemming the death toll.
In an August 26, 2020, article, the American Institute for Economic Research presented the following four “stylized facts” from the paper:26
1.“Once a region reaches 25 total COVID deaths, within a month the growth rate in deaths per day falls to approximately zero. In other words, no matter the country or state and its policies, deaths per day stop increasing within 20-30 days of passing a threshold of 25 deaths.
2.Once that happens, deaths per day either begin to fall or the trend remains flat.
3.The variability in death trends across regions has fallen sharply since the beginning of the epidemic and remains low. All states studied, all countries studied, have become more similar in their trends and have remained so.
4.Observations 1-3 suggest that the effective reproduction number, R, has hovered around one worldwide after the first 30 days of the epidemic.
The paper’s conclusion is that the data trends observed above likely indicate that nonpharmaceutical interventions (NPIs) — such as lockdowns, closures, travel restrictions, stay-home orders, event bans, quarantines, curfews, and mask mandates — do not seem to affect virus transmission rates overall.
Why? Because those policies have varied in their timing and implementation across countries and states, but the trends in outcomes do not.”
Lockdown Measures Should End Now
Put plainly, the measures we’ve endured these past six months were largely unnecessary. One key reason for why lockdown and social distancing measures had no impact, according to the researchers, is because “human interaction does not conform to simple epidemiological models.”
In a nutshell, human social networks overlap, allowing a virus to rapidly spread for a time. Then, the virus quickly loses momentum, as people have already been exposed via other social networks and are no longer susceptible. The end result is that a form of herd immunity develops, but at a lower rate of infection than typically assumed would be necessary.
What’s more, the authors argue that even if nonpharmaceutical interventions were at one point having some positive effect, that effect no longer applies. Therefore, it would be a mistake to include estimates of NPI effectiveness when trying to forecast the potential outcomes of relaxed measures. As reported by the American Institute for Economic Research:27
“This study provides strong statistical support for what so many have been observing for six months. The epidemic has a natural tendency to spread quickly at first and slow down, seemingly on its own, a point made not only here but as early as April 14 by Isaac Ben-Israel.28
Meanwhile governors imagine that very specific rules for opening bars and restaurants are the key to containment. Governments have conducted an unprecedented social, economic, and political experiment in controlling whole populations’ behavior, with high economic and human cost.
The authors ask the right question: has this experiment in government-managed virus control and suppression made a difference? The startling answer they found, after examining data from around the country and the world, is that the evidence simply is not there. If we are concerned about the evidence on this global experiment, we must concede that most government authorities have likely acted in error.”
Why Are They so Persistent With Mask Recommendations?
Considering the strong scientific evidence against it, why are governments so persistent in their recommendation of mask wearing? Clearly, for many, wearing a bandana or cloth mask provides a form of psychological defense, a way to feel less fearful because it feels like you’re doing something to protect yourself and others. But it’s a false sense of security.
Masks will not prevent you from exhaling or inhaling the aerosolized virus. Cloth masks are clearly also the least preferable option if you want to reduce the spread of infection, as their ability to block larger respiratory droplets is also limited.
In particular, N95 masks with airflow valves on the front should be avoided, as the valve lets out unfiltered air, thus negating the small benefit — the reduction in respiratory droplet emissions — you might get from a mask.29
But with mortality rates as low as they are, why would governments be pushing for a false sense of security? It seems completely unnecessary at this point. Remember back in March 2020 when they said we just need to slow down the rate of infection to avoid overcrowding hospitals?
How did we go from that to now having to wear masks everywhere until every trace of the virus has been eliminated, even though a vast majority remain asymptomatic and don’t even know they have the virus unless they get tested?
Overall, it’s starting to look as though mask mandates are being used as a psychological manipulation tool to encourage compliance with vaccination once a vaccine becomes available. At that point, I predict a tradeoff will be offered: Mask mandates will be dropped provided everyone gets vaccinated.
By then, many may be willing to take just about anything as long as they don’t have to wear a mask anymore. I would encourage you to read up on the many open questions relating to fast-tracked COVID-19 vaccines before making that decision. Overall, it seems the best way to avoid having to make such a devious trade is to engage in civil disobedience now, and go unmasked.
Analysis by Dr. Joseph Mercola

